Classification
By Shape:
Saccular: The most common type, balloon-shaped and connected to the artery by a narrow neck.
Fusiform: Characterized by a widespread dilation along a section of the artery.
Microaneurysms: Small in size and typically associated with hypertension.
By Size:
Small: Less than 10 mm
Large: Between 10–25 mm
Giant: Greater than 25 mm
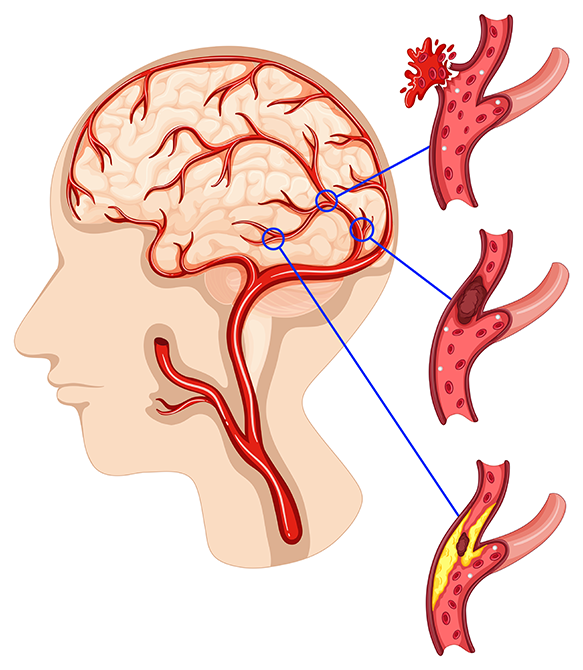
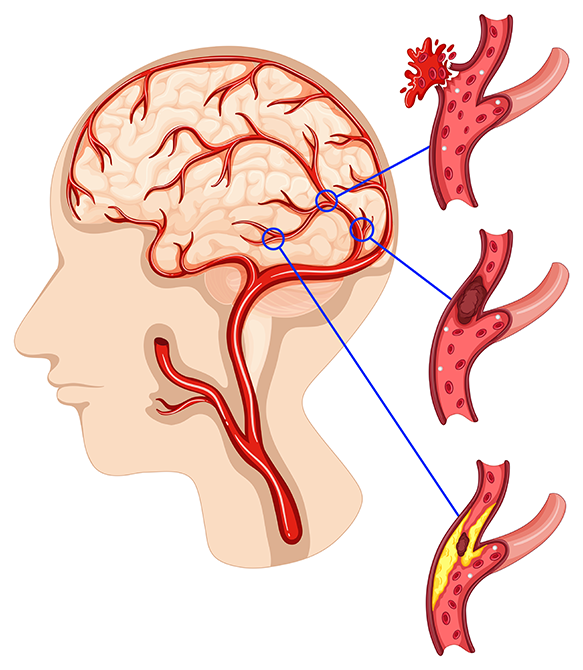
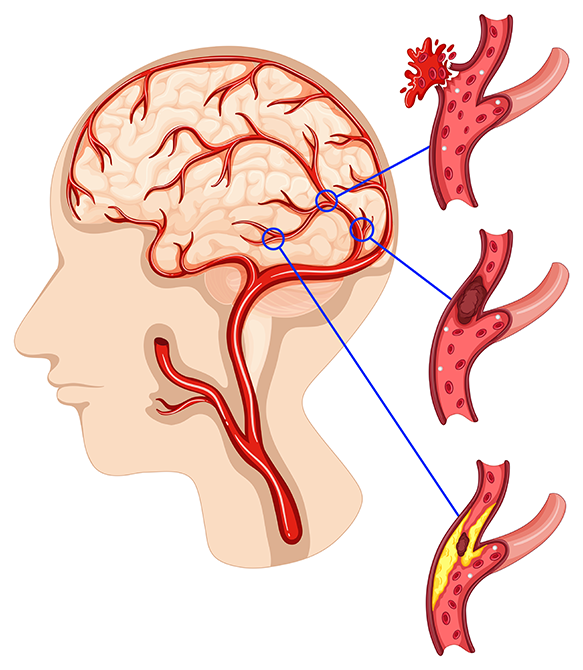
Risk Factors
Genetic Predisposition: A family history is a significant risk factor.
Chronic Diseases: Hypertension, atherosclerosis.
Lifestyle: Smoking, alcohol consumption.
Gender and Age: More common in women and individuals over the age of 40.
Symptoms
Unruptured Aneurysm:
Headache
Visual disturbances
Pain around the eyes
Neurological deficits (e.g., facial paralysis)
Ruptured Aneurysm:
Sudden and severe headache (often described as “the worst headache of my life”)
Nausea, vomiting
Loss of consciousness
Neurological impairments (paralysis, speech difficulties, etc.)
Diagnostic Methods
CT Angiography (CTA): Commonly used to visualize the aneurysm.
MR Angiography (MRA): Provides more detailed imaging.
Digital Subtraction Angiography (DSA): The gold standard for detailed evaluation of blood vessels.
Treatment
Surgical Clipping: A metal clip is placed on the neck of the aneurysm to stop blood flow into it.
Endovascular Treatment:
Coiling: Platinum coils are inserted into the aneurysm to promote clotting.
Stent or Flow Diverter: Devices used to redirect blood flow and reduce pressure on the aneurysm.
Medical Management: Monitoring unruptured aneurysms and controlling risk factors (e.g., managing blood pressure, quitting smoking).
Prognosis
Unruptured aneurysms can often be managed with careful monitoring, while ruptured aneurysms require emergency treatment. Complications following a subarachnoid hemorrhage (e.g., vasospasm, hydrocephalus) can significantly affect the outcome.